LEARN YOUR WAY: IN-CLASS┃HYBRID┃ONLINE
Strong personal support worker documentation is clear, factual, timely, and respectful. In long-term care, progress notes and charting help protect residents, support teamwork, and ensure changes in condition are addressed quickly and professionally.
Personal support work is hands-on, fast-moving, and deeply human. But behind the care you provide, helping someone dress, supporting mobility, assisting with meals, or offering reassurance, there’s another responsibility that matters just as much: documentation.
In long-term care, personal support worker documentation is part of safe care. It’s how the healthcare team stays aligned, how changes in condition are flagged early, and how resident needs are communicated clearly between shifts. It also protects you as a professional by showing what you observed and what actions you took.
This guide breaks down what PSWs should include in progress notes, how to keep charting objective, when to document changes or incidents, and the most common mistakes to avoid.
What Should a Personal Support Worker Include in Progress Notes?
In most long-term care settings, PSW progress notes should record information that another team member would need to safely continue care.
Progress notes often include:
- Relevant observations (mobility, appetite, mood, sleep, pain indicators)
- What care was provided (assistance with bathing, toileting, transfers, feeding)
- Resident response (tolerated well, refused, required extra support)
- Safety concerns (new bruising, unsteady gait, increased confusion)
- Follow-up actions taken (reported to nurse, documented refusal, monitored)
The goal is not to write a novel. It’s to chart what matters in a way that supports continuity of care and professional accountability.
What’s the Difference Between Objective Notes and Opinions in Documentation?
Objective documentation describes what you saw, heard, or did. Opinions describe what you think something means.
Objective charting sounds like:
- “Resident stated, ‘I feel dizzy when standing.’”
- “Resident refused breakfast and consumed approximately 25% of meal.”
- “Resident required two-person assist for transfer due to weakness.”
Opinion-based charting sounds like:
- “Resident was being difficult.”
- “Resident is exaggerating.”
- “Resident was lazy today.”
In PSW work, charting must stay respectful and factual. In many cases, your documentation may be reviewed by nurses, supervisors, family members, or legal professionals. Objective notes protect everyone involved.
If you’re thinking about your future in healthcare, you may also want to explore career options after PSW training.

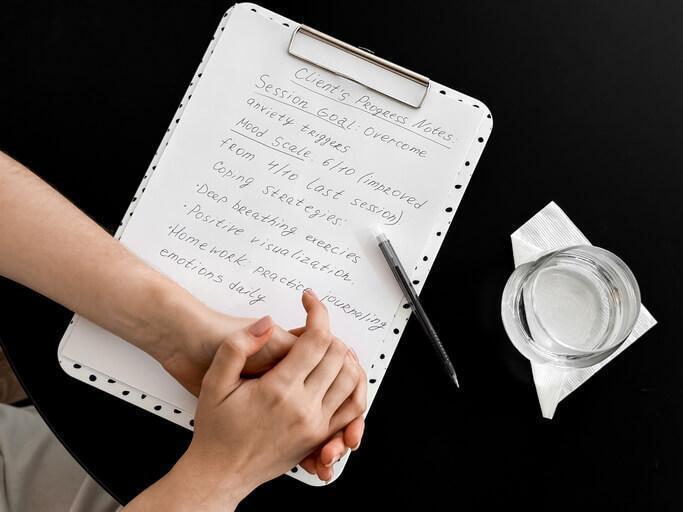
Personal support worker charting relies on objective observations, not opinions
When Should a Personal Support Worker Document a Change in Condition?
As soon as possible, especially when the change could affect safety or clinical decisions.
A “change in condition” can include:
- New confusion, agitation, or withdrawal
- Increased risk of falling or unsteady walking
- Unusual fatigue or weakness
- Sudden refusal to eat or drink
- New swelling, bruising, skin breakdown, or pain cues
- Shortness of breath or signs of infection
The most important part is this: documentation does not replace reporting. PSWs should document the change, but also communicate it immediately through the proper chain (usually the nurse).
How Do Personal Support Workers Document Incidents Safely and Professionally?
Incident documentation should be clear, time-based, and free of assumptions.
If something happens, such as a fall, injury, aggressive behaviour, or near miss, PSWs should document:
- What happened (facts only)
- Where and when it occurred
- What was observed immediately afterward
- What actions were taken (first aid, call bell, nurse notified)
- Any resident statements (quoted directly)
Avoid guessing causes. For example, instead of writing “Resident fell because the floor was slippery,” you would write “Resident slipped while walking from bed to bathroom. The floor appeared wet. Nurse notified.”
What Are Common Documentation Mistakes Personal Support Workers Should Avoid?
Some of the most common issues include:
- Charting late, after details are forgotten
- Using vague language (“seemed off,” “was fine,” “acting weird”)
- Including opinions or emotional judgments
- Failing to document refusals of care
- Documenting the wrong resident (a serious risk in busy settings)
- Leaving out follow-up actions (who you reported to, what you did next)
Another major issue is confidentiality. In Ontario, PSWs must follow PHIPA, which governs how personal health information is collected, used, and protected.
The Information and Privacy Commissioner of Ontario also provides guidance on how PHIPA is applied in real healthcare environments.

Progress notes should document changes in condition clearly and promptly
Why Documentation Is Part of Being a Strong PSW
In long-term care, documentation is not “extra.” It’s part of quality care. It supports resident safety, helps the team respond faster, and ensures everyone has the same information.
And for PSWs, it’s one of the clearest markers of professionalism. When your progress notes are consistent, objective, and complete, you become someone the healthcare team trusts.
If you’re exploring this career, you can learn more about what PSWs do across settings here.
How PSW Training Helps You Build Charting Confidence
Documentation is a skill, one that gets easier with structure and repetition. In our Personal Support Worker program, students learn how to chart objectively, follow workplace standards, and document incidents professionally.
Training also helps students understand the bigger picture: how PSW notes support nursing assessments, care planning, and resident outcomes. Over time, charting becomes less intimidating because you learn what matters, what doesn’t, and how to write in a clear professional voice.
Are you looking for a comprehensive Personal Support Worker program?
Contact Algonquin Careers Academy for more information.
Key Takeaways
- Personal support worker documentation supports continuity of care and resident safety
- Progress notes should include observations, care provided, and resident response
- Objective charting uses facts and quotes, not opinions
- Changes in condition should be documented promptly and reported immediately
- Incident documentation should be time-based, clear, and assumption-free
- PHIPA compliance and confidentiality are essential in long-term care
FAQ: Personal Support Worker Documentation
What should a personal support worker include in progress notes?
Progress notes should include relevant observations, care provided, resident response, safety concerns, and follow-up actions such as reporting to a nurse.
What’s the difference between objective notes and opinions in documentation?
Objective documentation describes what you saw, heard, or did. Opinions describe what you think something means.
When should a personal support worker document a change in condition?
As soon as possible, especially when the change could affect safety or clinical decisions.
How do personal support workers document incidents safely and professionally?
Incident documentation should be clear, time-based, and free of assumptions.
What are common documentation mistakes personal support workers should avoid?
Some of the most common issues include:
- Charting late, after details are forgotten
- Using vague language (“seemed off,” “was fine,” “acting weird”)
- Including opinions or emotional judgments
Social Media Messages
X (formerly Twitter)
PSW documentation is more than paperwork—it supports safety, continuity, and professional accountability. Learn the basics of progress notes in long-term care.
Facebook
Charting can feel intimidating at first. This guide breaks down what PSWs should include in progress notes—and how to write clearly and objectively.
LinkedIn
Clear, objective documentation is a core PSW skill in long-term care. Explore progress note basics, incident documentation tips, and common charting mistakes to avoid.
References
Government of Ontario – PHIPA (Personal Health Information Protection Act, 2004)
https://www.ontario.ca/laws/statute/04p03
Information and Privacy Commissioner of Ontario – PHIPA Guidance
https://www.ipc.on.ca/health-individuals/


